What is Bacterial Vaginosis
Bacterial vaginosis is a bacterial infection in the vagina. It occurs when the proportion of healthy bacteria is reduced in the vagina. The type of bacteria living in the vagina depends on its pH value. So, anything cause to change the balance of pH in vaginal can lead to the infection.
How does Bacterial Vaginosis Occur
Female reproductive age is from menarche to menopause. During this reproductive age, the vagina is lined by stratified squamous epithelium.
Usually, the vaginal pH range is between 3.5 and 4.5. Lactobacilli is a microorganism living in the vagina, which helps to maintain this pH range.
After the menopause, body estrogen level diminishes. It causes vaginal stratified squamous epithelium to atrophy. So the lactobacillus population decrease and the vagina is colonized by normal skin flora.
Growth and increase of the anaerobic microorganisms species and reduction of the lactobacilli in the vaginal flora cause this characteristic foul-smelling. Also, this increased pH up to 4.5 to 7 and become alkaline.
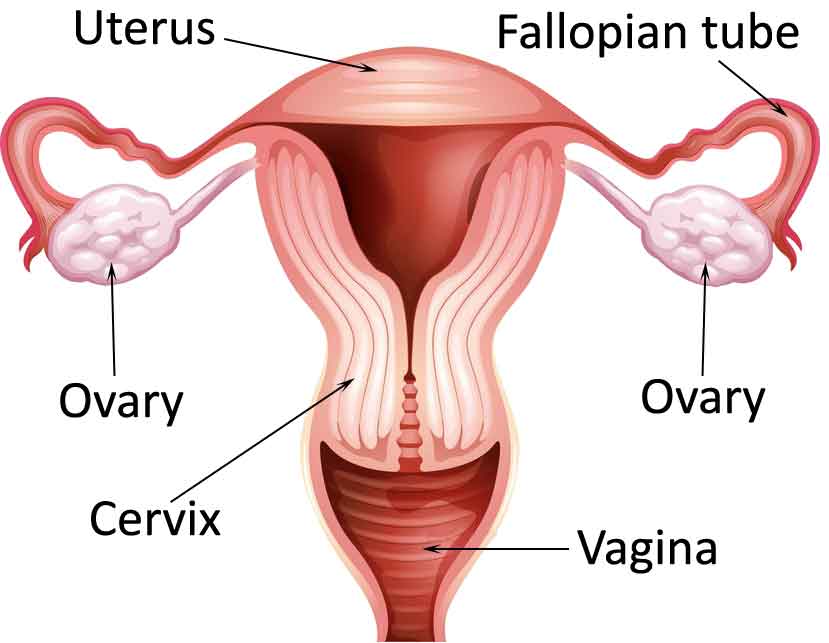
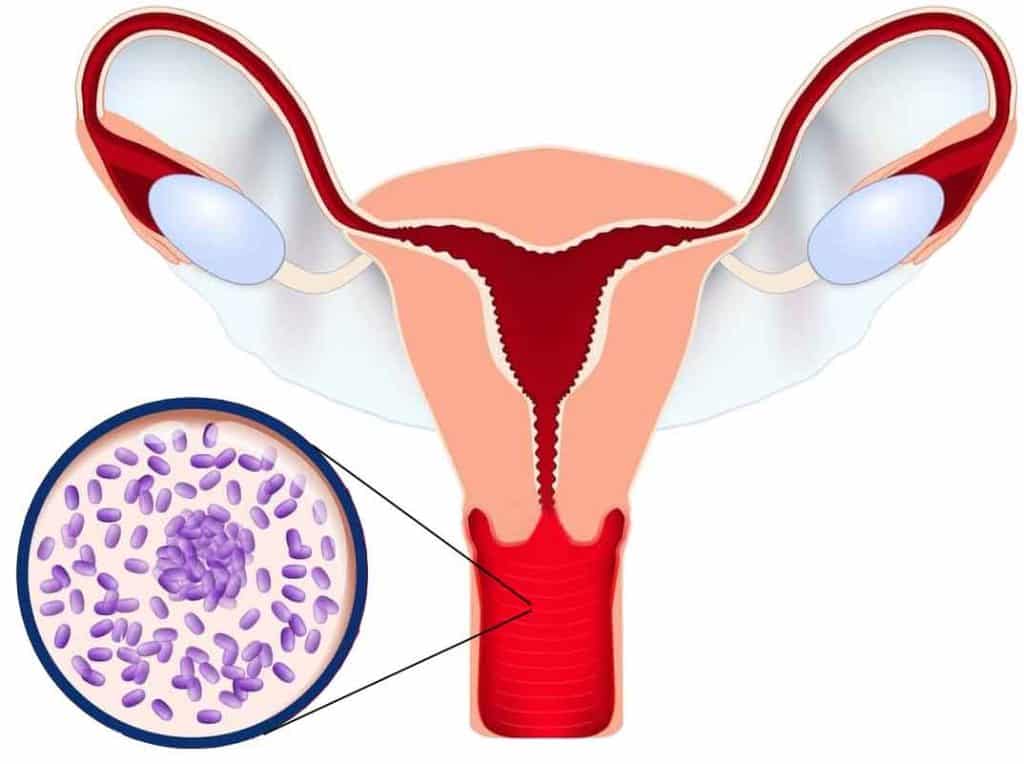
Infection in the vagina ascends to cause upward. So bacteria in the vagina, mount to the cervix, uterine tubes, and the fallopian tubes.
Risk factors for developing bacterial vaginosis
- Several risk factors are contributing to BV. Some of them are,
- Recent use of antibiotics,
- Sexual activity that leads to transmission,
- Wearing an intrauterine device,
- Decreased estrogen production,
- Douching
The incidence of bacterial vaginosis is increased when the number of sexual partners increases. Also, a recent change to a new sexual partner can increase the risk.
Male partners of the women who have BV have causative microorganism colonized urethra. But males do not show any signs or symptoms.
The causative organism for Bacterial Vaginosis
- The causative organism for bacterial vaginosis are,
- Gardnerella vaginalis
- Mycoplasma hominis
- Bacteroides species
- Mobilincus species
Signs and symptoms of Bacterial Vaginosis
It is a common condition for vaginitis, but there no inflammation in the vagina occurs.
- Fishy malodorous vaginal discharge.
- More prominent during and following menstruation.
- Creamy or greyish white vaginal discharge commonly adherent to the wall of the vagina.
- Asymptomatic carriers. (Asymptomatic carriers patients don’t show any signs and symptoms. But in their vaginas, Gardnerella vaginalis presence)
Diagnosis
- There are three types of criteria used for the diagnosis.
- Amsel criteria
- Hay/Ison criteria
- Nugent criteria
1. Amsel criteria
- To diagnose bacterial vaginosis, at least three of the following should be positive.
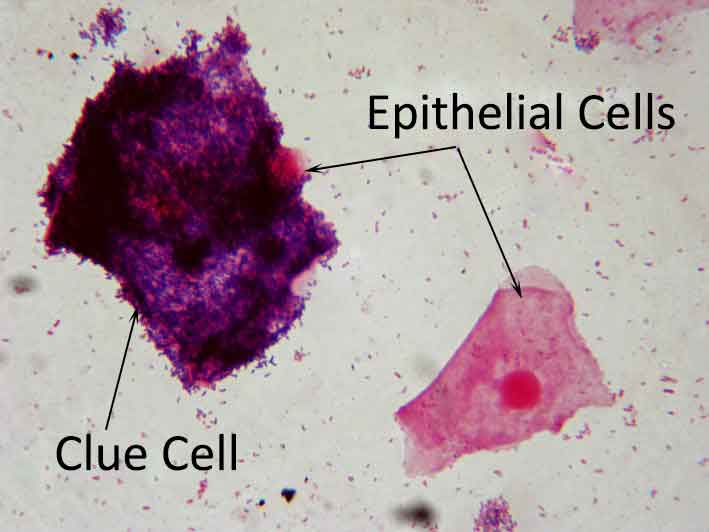
- Presence of clue cells on vaginal discharge when examined under the microscope.
- Clue cells are the epithelial cells which are covered with bacteria giving a characteristic stippled appearance under the microscopic view
- Creamy greyish white discharge from the vagina
- Vaginal pH value is more than 4.5
- Characteristic fishy odor release when adding alkali 10% KCl to vaginal discharge.
- Presence of clue cells on vaginal discharge when examined under the microscope.
2. Hay/Ison criteria
This method uses the presence of clue cells and gram variable coccobacilli to diagnose bacterial vaginosis.
Hay/Ison criteria are defined into three grades.
- Grade 1
- Lactobacillus is a predominance in vaginal discharge. So grade 1 is seen in healthy persons.
- Grade 2
- Lactobacillus is seen with the presence of Gardnerella and or Mobiluncus species. So grade 2 is considered an intermediate stage. Hence it is not diagnostic for bacterial vaginosis.
- Grade 3
- In vaginal discharge, Lactobacilli is absent or markedly reduced with a predominance of Gardnerella and Mobiluncus species. So grade 3 is diagnostic for bacterial vaginosis.
3. Nugent criteria
Nugent criteria use a score between one to ten. The score is based on the proportion of anaerobic species on vaginal discharge. For this test, trained microscopists are needed.
- Less than 4
- consider as a normal healthy
- Between 4 to 6
- consider as intermediate
- More than 6
- diagnostic for Bacterial vaginosis
Pregnancy and Bacterial Vaginosis
The pregnancy can divide into three trimesters.
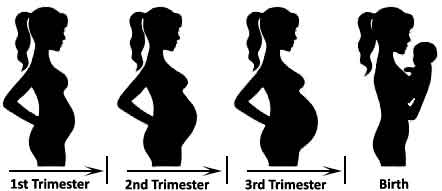
- The first week of pregnancy to the end of 12 weeks is the first trimester.
- The second trimester is from 13 weeks to 26 weeks.
- The third trimester is from 27 weeks to the end of the pregnancy.
Bacterial vaginosis affects the fetus according to the trimester. Usually, the effect occurs in the first trimester.
The first trimester affects lead to second-trimester miscarriage and preterm labor. Miscarriage is dying of the fetus or embryo before 20 weeks of the pregnancy. Preterm labor is labor happen after 20 weeks of the pregnancy and before 37 weeks of the pregnancy.
If pregnant women present with a previous history of second-trimester miscarriage or preterm labor, she should check for bacterial vaginosis, doing vaginal swab in early pregnancy. If bacterial vaginosis detects, it should treat the early stage of the second trimester.
Treatment for Bacterial Vaginosis
- There are two types of antibiotic treatments use for treating the BV.
- Metronidazole
- Clindamycin
Metronidazole is taken either orally or uses as an intravaginal gel. In both ways, the treatment period should be seven days. The intravaginal gel should apply at night, while oral metronidazole can use either as 400mg twice a day or as 2g daily.
Clindamycin is also taken either as an intravaginal gel or oral Clindamycin. If Clindamycin is taken orally, 300mg of it should use daily. Clindamycin can cause damage to the condom, no matter either it uses oral or intravaginal. Also, using Clindamycin can develop pseudomembranous colitis.