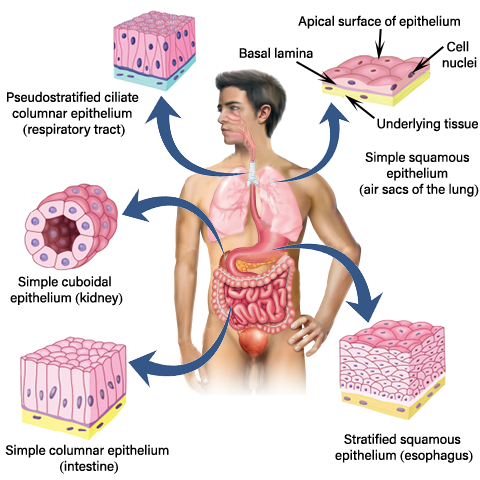
What Is an Ulcer
Break of the continuity of the epithelium tissue is known as an ulcer. Epithelial tissues perform essential functions in the body including,
- form the covering of all body surfaces
- line body cavities
- line hollow organs
Types of ulcer edges
Based on the ulcer’s edge, ulcers are categorized into different types. Therefore, it is better to have knowledge about the edges of ulcers.
- There are five types of distinguishable edges. They are,
- sloping edge
- punched out edge
- undermined edge
- rolled edge
- everted edge
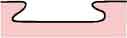
Sloping edge

- The edge is flat and gently sloping
- A sloping edge indicates that ulcer is healing
- So it isn’t shallow
- The new skin around the healing edge is pale and pink.
Punched out edge

- In the punched out edges, Rapid death is visible than the repair of the defect.
Rolled edge

- due to the slow growth, ulcer edge tissue and peripheral tissue becomes heaped-up.
- this is typically seen in basal cell carcinoma. (basal cell cancer)
- usually, the edge is pale pink or white
- telangiectases are commonly seen in the pale edge
Undermined edge
- In undermined edge, infection is in subcutaneous tissues of the ulcer than it is in the skin.
- So the edge becomes undermined.
Everted edge
- Ulcer edge is rapidly growing, and it spills out of the ulcer to overlap the normal skin.
Types of Ulcers
- Most common ulcers can be divided into three types. They are,
- Ischemic ulcers
- Neuropathic ulcers
- Venous ulcers
Treatments for ulcers are different according to their types.
Ischemic ulcer

The ischemic ulcers occur due to inadequate blood supply. So it can be seen in places where the blood supply is poor.
- This type is most common in elder patients who have,
- Cerebral vascular disease (ischemic stroke)
- Coronary vascular disease (heart attack)
- When artery obstructs, the blood supply to following places gets poor causing Ischemic ulcers
- the tip of the toes and fingers
- over the pressure points
Causes for ischemic ulcers
- There are 2 causes,
- Large artery obliteration
- e.g. Atherosclerosis
- e.g. Embolism
- Small artery obliteration
- e.g. Diabetes Mellitus
- e.g. Scleroderma
- e.g. Prolonge applied local pressure
- e.g. Radiation
- e.g. Trauma
- e.g. Elective burns
- e.g. Burgers disease
- e.g. Athero embolism
- Large artery obliteration
How to identify ischemic ulcers
- The size of ischemic ulcers varies from small to very deep and large.
- It is elliptical.
- Surrounding tissue and ulcers are very tender.
- Ischemic ulcers are excruciating, and pain increases while resting (while sleeping).
- After removing the dressing which applied to the ischemic ulcer, pain persists for hours.
- It does not bleed but has a thin serous discharge, and that discharge may be purulent.
- Surrounding tissues of the ischemic ulcers are cold due to poor blood supply (ischemic).
- These ulcers are indolent and slowly get deeper and then become larger. So they are very deep, and it penetrates deep fascia, tendon, bone, and occasionally even to joints.
- The base of the ulcer cover with grey, yellow slough.
- Near the ulcer, the arterial pulse does not feel because above the ulcer, arterial occlusion occurs.
- Since surrounding tissue is ischemia, infection in the ulcer does not spread. So local lymph nodes do not enlarge in ischemic ulcers.
Treatment for the ischemic ulcers
- The main essential need is the restoration of blood supply. It can be done by,
- Angioplasty
- In angioplasty, occlude in the artery is removed via inserting a thread and thin tube through blood vessels to the occluded site. Then the cause of the occlusion is grabbed and removed.
- Bypass artery
- A blood vessel is taken from another area of the body, and it is used to bypass the occluded arteries.
- Endarterectomy
- It is a surgical procedure to remove the atheromatous plaque material or block. Plaque removal is doing by surgical excision of the artery, and then it is closed.
- Angioplasty
- After restoring blood supply, treat the ulcer as usual by doing wound toilets ( removing slough and dead debridements) and keeping appropriate moisture to the ulcers. Also, it is important to give suitable antibiotics to promote healing.
Neuropathic ulcers

Neuropathic ulcers can occur in pressure points. When prolonged pressure continuously applying to the tissues at pressure points, tissues become ischemic.
Ischemia is painful. Usually, when the pain feels to a person, he tends to change the posture. But when pain sensation is lost, the person does not change the position. So the compressed tissue becomes permanently damaged due to ischemia. This ultimately leads to neuropathic ulcers.
Causes of neuropathic ulcers
- Peripheral nerve lesions.
- Diabetes Mellitus
- Nerve injury
- Leprosy
- Spinal cord injury
- e.g. Spina bifida
- e.g. Tabes dorsalis
- e.g. Syringomyelia
How to identify Neuropathic ulcers
- Neuropathic ulcers are deep and penetrating ulcers
- It occurs in the pressure points
- Surrounding tissues are healthy, and they have a good circulation
- All arterial pulses near the wound are present, but the pain sensation completely lost.
- So it is painless.
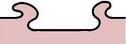
Treatment of neuropathic ulcers
The main focus in the neuropathic ulcer treatment is to reduce pressure on the affected area.
1. Therapeutic shoes
When the foot has this type of ulcer, therapeutic shoes are recommended to use. It helps to reduce the risk of ulceration by reliving mechanical pressure.
2. Surgery for correct foot deformities
Surgery is another option to remove excessive pressure cause by deformed foot in ulcer area. After the surgery, it is a must to cleaning, and dressing the wound.
Venue ulcers
Venous ulcers occur as a result of venous valves malfunction. Venous valves help to prevent the backflow of blood. When valves are malfunctioning, blood falls under gravity and accumulate in leg veins. Since increased pressure leads to vain rupture, this causes to create an open wound.
Most of the patients with venous ulcers do not have visible varicose veins. But 50% of venous ulcer patients have varicose veins. Remain 50% of patients develop ulcers due to post-thrombotic deep vein damage.
- The venous ulcer usually occurs,
- after the age of 40, with suffering many years of venous disease
- in young adults due to post-thrombotic disease
- in children and teenagers due to congenital venous malformations
- commonly in females than males
How to identify a venous ulcer
- Before the ulcers develop, patients experience aching pain, discomfort, and tenderness over the skin for many years.
- Many venues ulcers are painless. But some can be painful.
- Ulcer discharge gives terrible smelling.
- Due to the smelling, patients are subject to social isolation and even depression.
- Some time itching and scratching lead to creating an ulcer.
- Ulcers can be in many shapes and sizes.
- Edge is gently sloping when it begins to heal. Pink color new epithelium migrates to its surface.
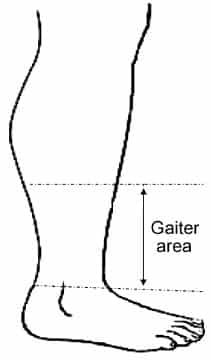
- Mostly venous ulcers are common in the gaiter area medial aspect of the lower limb.
- Venous ulcers are shallow and flat
- Discharge is purulent with serous and some time bloodstained.
- Surrounding tissues usually show signs of chronic venose hypertension, such as tenderness, pigmentation, inflammation, induration.

There are dilated intradermal and subcutaneous veins. Venous ulcers can be considered as colonized rather than infected. Since they are not infected lymph node does not enlarge and tender due to the venous ulcers.
Types of venous ulcers
- There are two types of venus ulcers. They are,
- Acute venous ulcer
- Chronic venous ulcer
Acute venous ulcer
- Surrounding lipodermatosclerosis is clearly visible.
- Tissues are dying and sloughing. It is very painful.
Chronic venous ulcer
- The base contains small healthy granulation tissue.
- But mostly avascular fibrous tissue base is fixed to the deep tissue and exposed tendons and healing ulcer.
- Surrounding skin looks healthy.
- The base of the ulcer is clean and pink, and the edge of the ulcer is sloping by making new epithelium.
Complications of chronic venous ulcer
- It can lead to squamous cell carcinoma.
- In there it edges are raised and thickened, and inguinal lymph glands became enlarged.
Treatment for the venous ulcer
- Treatment of venous ulcer is combined with,
- wound dressing,
- topical applications,
- debridements,
- systemic therapy,
- compression therapy,
- sclerotherapy and
- supportive therapy
Dressing
- Irrigation of wound with normal saline
- The dressing should be nonadherent dressing with zinc oxide. It promotes epithelialization.
Topical treatment
- Use topical antibiotics on the wound
Systemic therapy
- Systemic antibiotics should only be given in a condition of the infection, and it should not use for bacterial colonization in the wound.
Compression therapy
- The multi-layered high compression system with adequate padding is the first-line therapy for venues ulcer.
- High compression cause to better healing. The compression pressure should be preferably in the range of 30-35 mmHg.
Sclerotherapy
- Sclerotherapy is given when superficial varicosities present near the venous ulcer.
Supportive therapy
- Improve nutrients
- Elevate the wound site (Wound site swelling will reduce)
- Exercise to feet (Exercise improves muscle function. So it helps to pump blood in veins towards the hearts)
Untreated ulcers can be lead to amputations of the limbs. So it should not be taken lightly.

Pingback: Bacterial Vaginosis - MedFog - Public Awareness Towards Healthy Lifestyle
Pingback: What is Menorrhagia - Symptoms, Causes, Diagnosis and Treatment
Pingback: Anal Fissure - Causes - Symptoms - Treatment - MedFog
Pingback: Lansoprazole - Drug Information - Side effects - MedFog